 |
Management of Rh negative pregnant women
|
|
|
|
Management of Rh negative pregnant women
Management of the Rh-negative, non-sensitized pregnant woman
The main goal of management is prevention from producing RH+ antibodies. Indirect antiglobulin test (IAT) must be performed in all pregnant women who are Rh negative, at terms 20, 24, 28 weeks of pregnancy. Women found to be Rh-negative with a concurrent negative antibody screen are not alloimmunized and thus are candidates for anti-D IgG prophylaxis. (Fig. 177) Anti-D immunoglobulin can prevent R-negative non-sensitized mother from producing anti-D antibodies when exposed to R-positive (D-positive) blood. All Rh - negative women (who have not actively formed their own Anti-D antibodies) should be offered Rh0(D) immune globulin in the following clinical situations:
1. First trimester (dose 250 IU):
· Chorionic Villus Sampling;
· Miscarriage;
· Termination of pregnancy (either medical or surgical);
· Ectopic pregnancy.
2. Second and third trimester (basic dose 625 IU):
· Obstetric haemorrhage;
· Amniocentesis, cordocentesis;
· External cephalic version of a breech presentation, whether successful or not;
· Abdominal trauma,
· any other suspected intra-uterine bleeding or sensitising event.
In general, in case of uncomplicated course of pregnancy in non-sensitized mother a dose of 300 microgram of Rh0(D) immune globulin is useful at term 28 weeks of pregnancy to prevent immunization in pregnancy and decreases risk of sensitization. In some countries (Australia and New Zealand) all Rh (D)-negative women (who have not actively formed their own Anti-D) should be offered a prophylactic dose of Rh0(D)IgG again at approximately 34 weeks gestation.
Postpartum if the antibody screen is negative a second dose of Rh0(D)IgG is given if the infant is Rh-positive. The second dose of Rh0(D)IgG (300 µg) should be entered within 72 hours after delivery.
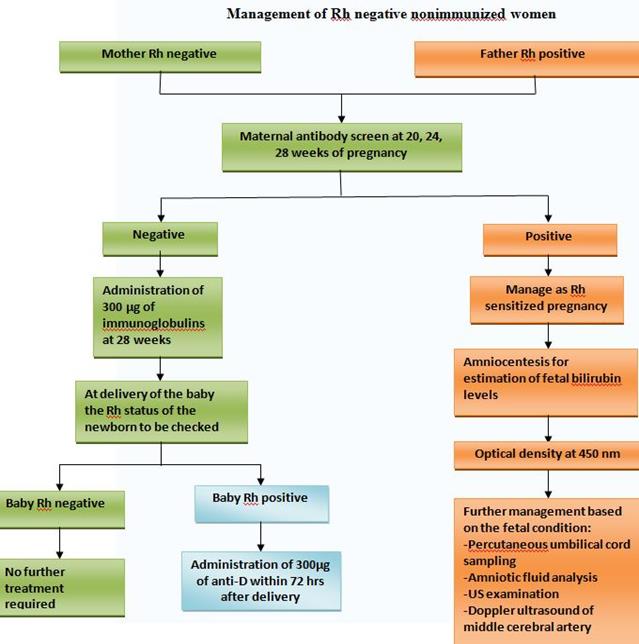
Fig. 177. Management of Rh-negative patient
Evaluation of immunized patient
The history taking and special examination can help to predict the severity of Rh-incompatibility and hemolytic disease of the fetus.
A detailed evaluation should include:
Management of the Rh-negative, sensitized pregnant women
Women who are Rh- negative with a concurrent positive antibody screen are considered to be alloimmunized to a red cell antigen(s) (assuming she has not recently received anti-D IgG), and should then undergo identification of the antigen(s) as well as determination of antibody titers to the specific antigen(s) to guide pregnancy management.
1. In general, women with titers higher than 1: 4 should be considered Rh alloimmunized. Titers tend to correlate more reliably with the severity of fetal disease in the first sensitized pregnancy than in subsequent pregnancies. These are usually performed monthly until 24 weeks of gestation, after which time titers should be repeated every 2 weeks. If titers remain below the critical titer, delivery can occur at term. A critical titer is defined as the titer associated with a significant risk for fetal hydrops. Usually, pregnancies in which antibody titers are 1: 8 or lower can be managed by serial monitoring of maternal antibody titers.
|
|
|
2. Once the titer of maternal antibody reaches the level greater than 1: 16, the fetus has a 10% risk of dying in uterus. In general, the management is as follows:
· IAT titers of < 1: 32 or less are managed noninvasively with repeat antibody titers every 2 weeks.
· IAT > 64 serial amniocentesis (every 2 to 3 weeks).
· IAT titers of > 1: 32 with pregnancies at greater than 27 week are usually monitored with serial amniocentesis
· If the father is heterozygous (Dd) or his blood is unavailable then fetal blood sampling by cordocentesis (aka as percutaneous umbilical cord blood sampling, PUBS) or amniocentesis may be used to determine the fetal Rh (or atypical antigen) status if the IAT titer is > 1: 32 or albumin titer > 1: 16.
3. Serial Amniocentesis
Fetuses affected by hemolytic disease secrete abnormally high levels of bilirubin into the amniotic fluid. The amount of bilirubin can be quantitated by spectrophotometrically measuring absorbance at the 450-nm wavelength in a specimen of amniotic fluid that has been shielded from light. Alternatively, percutaneous umbilical blood sampling (PUBS) may be used to determine all blood parameters directly. If amniocentesis is used to monitor the fetus, the results (delta 450) are plotted on a " Liley" curve. (Fig. 178)
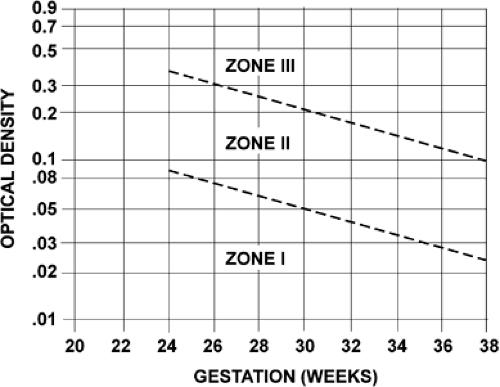
Fig. 178. " Liley" curve.
The degree of fetal hemolytic disease according to the level of amniotic bilirubin may be evaluated is as follows (Table 24)
|
|
|


