 |
Evaluation of degree of fetal hemolytic disease depending on optical density of bilirubin
|
|
|
|
Table 24
Evaluation of degree of fetal hemolytic disease depending on optical density of bilirubin
| Optical density of bilirubin (450 nm) | Bilirubin content in amniotic fluid | Fetal state (condition) |
| 0, 15-0, 20 | 0-2, 8 | Low risk (the 1st degree or no hemolytic disease). Fetuses in zone I are usually followed with amniocentesis every 3 weeks. |
| 0, 21-0, 34 | 2, 9-4, 6 | Risk is moderate (2nd degree). Fetuses in low Zone II are usually followed by amniocentesis every 1-2 weeks. |
| 0, 35-0, 70 | 4, 7-9, 5 | High risk for fetus (3rd degree). Fetuses require transfusion or delivery |
| > 0, 70 | > 9, 5 | Very high risk (risk of fetal death) |
3. Direct examination of blood samples of a fetus by obtaining blood from umbilical cord, named fetal blood sampling (cordocentesis, or PUBS) under the ultrasonic control, including:
· - Hemoglobin and hematocrit levels;
· - Direct Coombs’ titer (antibodies attached to fetal red cells)aka direct antiglobulin test (DAT );
· - Bilirubin level;
· - Reticulocyte count;
· - Serum protein levels.
4. Real time ultrasound. Several studies have shown that serial ultrasound is not an accurate method of assessing the degree of fetal anemia. Polyhydramnios may be the earliest sign of significant fetal anemia, but it is not always present. The ultrasonic signs of significant forms of hemolytic disease are: hyperplasia of the placenta (it can reach 50 mm in thickness), increase of fetal abdominal size (ascites), fetal hepatomegaly and hypersplenism, edematous circuit of the fetal head.
Ultrasound should therefore be used as an additional tool and cannot replace amniocentesis, cordocentesis.
Lastly, in women with extremely high titers (> 256), at less than 28 weeks, where the fetus does not demonstrate hydrops, and there is a documented history of fetal death due to hydrops intravenous immune serum globulin (IVIG) might be offered. The dose is 400 mg/kg per day for 5 days, with repeat infusions every 15 to 21 days. Specific contraindications to intravenous immunoglobulin use include a previous episode of intravenous immunoglobulin-induced anaphylaxis (rare) and selective IgA deficiency
5. The study of peak systolic velocity in the middle cerebral artery (MCA) can be used to detect moderate and severe anemia in nonhydropic fetuses. Because of fetal anemia results in decreased blood viscosity, the peak systolic velocity (PSV) of blood flow results increased in case of anemia. Study of MCA is preferred as it can be evaluated using a minimal angle of insonation. Generally, a value of 1. 5 multiples of the median (MoMs) is considered critical in establishment the timing of fetal blood sampling. Serial MCA Doppler studies are obtained every 1-2 weeks depending on the trend. Once the MCA Doppler peak systolic velocity (MCA-PSV) reaches more than 1. 5 MoMs for gestational age (or the delta OD450 measurements have entered high zone 2 or zone 3, or the fetus has been diagnosed with hydrops based on ultrasonographic findings), a decision should be made to perform an PUBS with possible intrauterine blood transfusion (IUBT) if the hematocrit is less than 30%. Alternatively, if beyond 34 weeks' gestation, the decision is to proceed towards delivery (32 wk with mature lung indices).
|
|
|
6. Fetal blood sampling (FBS) by cordocentesis (aka as PUBS), is the only definitive approach in diagnosing of fetal anemia and acidosis by direct measurement of the fetal hemoglobin and acid-base status. When fetal hematocrit is less than 30%, the only therapeutic option is intrauterine fetal transfusion. (Fig. 179) The source of red cells for intrauterine transfusion is typically a blood type O, RhD-negative, cytomegalovirus- negative donor. This prosedure is meant to keep the fetus viable until he or she is mature enough to be delivered. The purpose of intrauterine transfusion is to maintain the fetal Hb value at more than 90g/L. Intrauterine fetal transfusion may be done either intraperitoneally or intravascularly (through fetal umbilical vein). Intravascular transfusion instantly increases fetal hematocrit and Hb, whereas intraperitoneal transfusion requires the fetus to absorb transfused blood through the lymphatic system (need time). The timing of repeat procedures is based on fetal hematocrit and usually occurs within 2 to 3 weeks. Serial intrauterine transfusions, if required, are usually performed until 34 weeks’ gestation, because after this time the risk of the procedure is greater than benefits.
7. In determining the optimal delivery time, gestational age, severity of fetal anemia, and fetal lung maturity should all be considered. If fetal surveillance remains reassuring (MCA-PSV value < 1. 5 MoMs or spectrophotometric analysis does not indicate severe fetal hemolytic anemia), labor should be induced at 37-38 weeks of gestation. If fetal surveillance is not reassuring delivery should be planned after confirmation of fetal lung maturity.
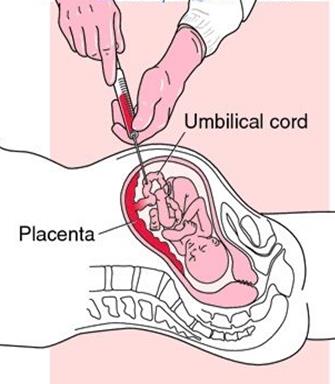
Fig. 179. Intrauterine blood transfusion (intravascular procedure).
|
|
|


