|
Amniocentesis
|
|
|
|
The child develops in the womb for 9 months, being in the amniotic cavity (SYN.: bag of water, bag of membranes, etc) within which the child lives. Amniotic fluid surrounds the fetus and is composed of nutrients, which saturate the fetus, and his/her waste products. Amniotic fluid is a clear, pale yellow fluid that:
- Protects the fetus from injury
- Protects the fetus against infection
- Allows the baby to move and develop properly
- Helps control the temperature of the fetus.
Amniotic fluid contains fetal cells - cells that the skin of the developing baby has shed). Each cell in the fluid contains their complete set of DNA (genetic information). Analyzing these cells helps to assess the fetus' health and detect any potential problems. In some cases when ultrasound and other research methods are unable to identify obvious pathology, which can endanger the life and health of the fetus, amniocentesis is assigned to one of the most sophisticated prenatal procedures.
Amniocentesis is a biochemical study of amniotic fluid to detect oxygen starvation of the fetus and determine the defects of its development. Amniotic fluid (3 to 30 ml) obtained by puncture of the anterior abdominal wall, uterus and amniotic membrane. A sample of the amniotic fluid is collected using a needle and a syringe. The first diagnostic amniocentesis was carried out in 1966. A decade earlier fetal cells and sex chromatin has been identified in the amniotic fluid. Until that time, the puncture of the amniotic sac was used in the nineteenth century as a method of treatment of polyhydramnios, and also with purpose of aborticide at late terms of pregnancy.
The essence of amniocentesis consists in taking of amniotic fluid to determine fetal karyotype and confirm the suspected diagnosis, such as:
1. Down syndrome - chromosomal abnormality, in which the karyotype has an extra copy of genetic material on the 21st chromosome, i. e. there is trisomy of chromosome 21 (trisomy 21). Phenotypic characteristics of Down' syndrome presented with brachycephaly, flat face and occiput, Mongoloid slitty eyes, epicanthus, a skin fold on the neck, shortening of limbs, brachydactyly, transverse palmar fold, etc.
Down syndrome can be determined in utero (by ultrasound, chorionic villus sampling, amniocentesis, cordocentesis), or after birth (based on phenotypic characteristicsand genetic studies). Children with Down syndrome are need in correction of related developmental disorders (Fig. 93, 94).

Fig. 93. A child with Down syndrome

Fig. 94. A child with Down syndrome
Down syndrome is autosomal syndrome, in which the karyotype has 47 chromosomes due to an extra copy of 21-th pair of chromosomes. Down syndrome is logged with a frequency of 1 case per 500 to 800 newborns. The sex ratio among children with Down syndrome is 1: 1. Down syndrome was originally described in 1866 by English pediatrician L. Down, but the chromosomal nature and essence of the pathology (trisomy 21) was identified almost a century later.
|
|
|
Clinical symptoms of Down syndrome range from congenital malformations and to secondary immunodeficiency. Children with Down syndrome need extra medical care from various specialists, therefore they constitute a special category in Pediatrics;
Clinical symptoms of Down syndrome varied from congenital malformations and mental retardation to secondary immunodeficiency. Babies with Down syndrome require additional medical care from various specialists, thus they are a special category in Pediatrics;
2. The Patau syndrome is a chromosomal condition caused by the presence of additional copies of the 13th chromosome (trisomy 13). Typical characteristics of Patau syndrome are multiple defects of the nervous system (microcephaly, holoprosencephaly), eyes (microphthalmia, cataract), musculoskeletal system (polydactyly, cleft lip and palate, omphalocele), heart, urogenital system and others. Such severe developmental abnormalities are the cause of frequent cases of intrauterine fetal death and low life expectancy of children with this disorder. To identify and confirm the Patau syndrome, prenatal screening is carried out, and the study of the karyotype of the child after birth. Children with Patau syndrome need in restorative therapy, and correction of congenital malformations (by indications) (Fig. 95. ).

Fig. 95. Baby with Patau syndrome
Fig. 96. Baby with Patau syndrome
Patau Syndrome is also known as The D trisomy syndrome and trisomy 13. The frequency of children, born with Patau syndrome, is 1: 7000-10000; the sex ratio is approximately 1: 1. The clinical syndrome has been described in the XVII century; the correlation between the disease and chromosomal pathology was established in 1960 by K. Patau, after whom the syndrome got its name.
3. Edwards syndrome - also known as trisomy 18, is a genetic disorder caused by the presence of all, or part of a third copy of chromosome 18, and is accompanied by multiple malformations. Edwards syndrome is characterized by peculiar phenotypic features: dolichocephalism, microphthalmia, auricular hypoplasia, etc. ), anomalies of the musculoskeletal, cardiovascular, digestive, genitourinary system, central nervous system (Fig. 97).
Currently most cases of trisomy 18 are prenatally diagnosed, based on screening by maternal age, maternal serum marker screening, detection of sonographic abnormalities during the second and third trimester. It can also be diagnosed after birth (based on external characteristics and cytogenetic studies). Children with Edwards syndrome are in need of symptomatic treatment and good care. (Fig. 97)

Fig. 97. Newborn baby with Edwards syndrome
The first reported infants were described in 1960 by Edwards, who identified more than 130 typical for this pathology symptomatic defects, and after whom the syndrome got its name.
Edwards syndrome is the second most common chromosomal disorder after down's syndrome; the frequency of birth of children with Edwards syndrome is 1 in 5000-7000. About three quarters of all patients with Edwards syndrome girls; it is assumed that the majority of pregnancies with a male fetus ends in fetal death and spontaneous abortion;
4. Diseases, caused by abnormalities of the neural tube development of the fetus - a number of birth defects. Congenital malformation developments are one of the main causes of child mortality and disability. A significant place in this pathology occupy the defects of the neural tube, which form a variety of disorders of the nervous system from defects of the spine and spinal cord to anencephaly.
|
|
|
In case of gross defects of neural tube (anencephaly, complete cleft spine, etc. ) the fetus dies in utero, or is born nonviable and die in the next few hours or days after birth. Therefore, social and medical aspects of the rough neural tube development defects are reduced to the prevention of the formation of the defect, its early diagnosis and abortion. Therefore, social and medical aspects of the severe neural tube development defects are reduced to the prevention of the formation of the defect, its early diagnosis and termination of pregnancy.
Other problems arise when less serious violations of the formation of the spinal cord and spine (united by the concept of spinal dysraphia, or defects in neural tube development), which in foreign literature are united by the term spina bifida (Fig. 98);


Fig. 98. Children born with defects in neural tube development
5. Cystic fibrosis;
6. Sickle cell disease (SCD) and its variants are genetic disorders resulting from the presence of a mutated form of hemoglobin. The most common form of SCD found in North America, it is homozygous HbS disease (HbSS), an autosomal recessive disorder first described by Herrick in 1910. SCD causes significant morbidity and mortality, particularly in people of African and Mediterranean ancestry.
Sickle cell anemia is caused by a specific genetic mutation in the β globin gene which causes polymerization of hemoglobin under deoxygenated conditions. The polymers distort the red cell’s shape into a crescent or sickle shape (Fig. 99). The shape prevents normal blood flow through capillaries and increased adhesion to endothelial cells. Decreased blood flow leads to tissue infarction and a wide range of clinical symptoms, the hallmark of which include splenic infarction and painful episodes termed vasooclusive crises.

Fig. 99. Red blood cell in sickle cell syndrome
Infection, bone marrow aplasia, or lung involvement (acute chest syndrome) can develop acutely and be fatal. Anemia is present, and sickle cells are usually evident on the peripheral smear. SCD is present mostly in blacks. It also is found, with much less frequency, in eastern Mediterranean, India and the Middle East populations. The incidence of SCD depends on prevalence of malaria (an infectious disease that affects human red blood cells).
Due to population migration and mixing of ethnic groups today, this type of anemia can occur in people of any race in various regions of the world. Men and women suffer equally often.
Amniocentesis is also performed to detect complications of the current pregnancy, including intrauterine infection, fetal hypoxia.
In some cases, when preterm delivery is indicated, amniocentesis is used to assess maturity of fetal lung, for reduction of the volume of amniotic fluid when polyhydramnios, to make an antenatal treatment for the fetus.
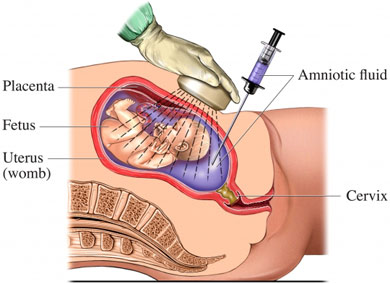
Fig. 100. Amniocentesis’ Procedure.
Amniocentesis is invasive (i. e., penetrating the natural barriers of the body: skin, mucous membranes) procedure, performed in different stages of pregnancy, (Fig. 100). It is puncture of amniotic sac, in order to:
• obtain amniotic fluid for laboratory examination;
• conduct amnioreduction - pumping of amniotic fluid, if there are too many (so-called polyhydramnios);
• pour medicines for abortion in the II trimester;
• pour medicines into the amniotic cavity if necessary for treatment;
This procedure is quite specific, and, therefore, the term of pregnancy, in which it is conducted, is of great importance. The best option is term of pregnancy from 16 to 20 weeks. Depending on the pregnancy term, and what tools are used (Fig. 101), several types of amniocentesis procedure distinguished.
|
|
|
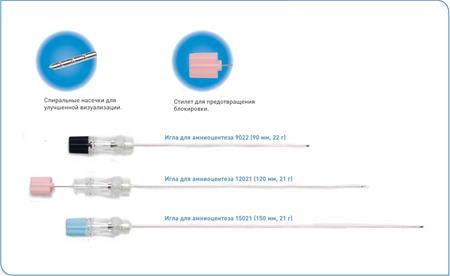
Fig. 101. Tools for amniocentesis
Types of amniocentesis by terms of pregnancy
• early: performed in the first trimester of pregnancy (from 8 to 14 weeks);
• later: assigned after the 15th week.
Types of amniocentesis by technology of procedure:
• use a needle adapter that allows you to make a more accurate puncture, without affecting the nearby tissues;
• the method of " free hand" when the needle directs the physician.
|
|
|