|
Calculating the Expected Date of Delivery (E.D.D.) 4 страница
|
|
|
|
Fig. 127. Shredder sign of placental separation: 1 – uterus fundus after delivery of a fetus; 2 – height of standing of the uterus fundus after separation of the placenta, 3 - height of standing of the uterine fundus after the birth of the afterbirth.
2. Alfeld sign. After the separated placenta has descended into the lower segment of the uterus or into the vagina, the outer segment of the umbilical cord extends. To observe this symptom, it is necessary immediately after the birth of the baby to apply the Kocher clamp or ligature to the umbilical cord at the level of the pudendal cleft. After detachment and descent of the placenta, the clamp is lowered at a distance of 10-12 cm from the pudendal cleft. (Fig. 128)

Fig. 128. Alfeld sign
3. Custner sign. Pressing down the symphysis pubis with the palm results in protruding of the external umbilical cord. If the cord is not protruded, or becomes shorter, it means that the placenta has not separated yet. (Fig. 129)
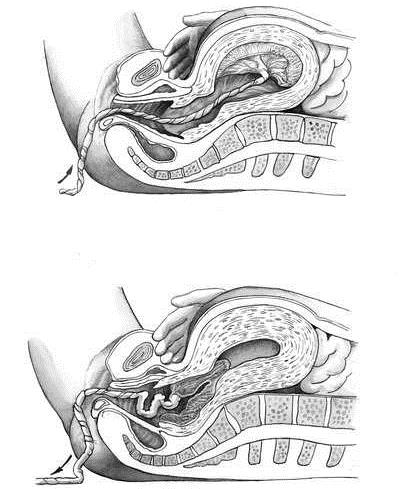
Fig. 129. Custner sign.
4. Strassmann sign is one of the most reliable and is checked as follows: standing on the side of the mother, it is necessary to take the cord with one hand above the clamp and squeeze it lightly. The second hand produces a slight flickering over the uterus in various parts of it. If the placenta is still connected to the wall of the uterus, the effleurage of the uterus by the blood filling the intervillous spaces is transferred to the contents of the capillaries of the villi, and of them - the blood filling the vein of the umbilical cord. The hand holding the umbilical cord will feel a slight push - fluctuation. With the separated placenta, there is no fluctuation. Low abdominal bulge — placenta separates and is situated in the lower segment.
After the separation of the placenta it will be expelled easily. Sometimes, the separated placenta may stay too long in the uterine cavity. Only when the features of the placental separation are confirmed, the patient is asked to make an effort like during the fetus birth. The increased inter-abdominal pressure is often adequate to expel the placenta. If the patient fails to expel it, one can wait safely up to 10 minutes if there is no bleeding. As soon as the placenta passes through the introitus, the hands and twisted round and round with gentle traction grasp it so that the membranes are stripped intact. If the membranes threaten to tear, they are caught hold of by sponge holding forceps and in similar twisting movements the rest of the membranes are delivered. A small bit of the torn membranes may be left inside, but a large one (2/3 and more parts) if left inside may lead to complications (bleedings, septic endometritis).
If the spontaneous expulsion fails, any one of the following methods can be used to expedite expulsion.
Folding of the anterior abdominal wall with two hands and asking the patient to make an effort. (Abuladze’s method) (Fig. 130).
|
|
|

Fig. 130 Abuladze method
Pressing the angles of the uterus with two fists (Henter’s method) (Fig. 131).
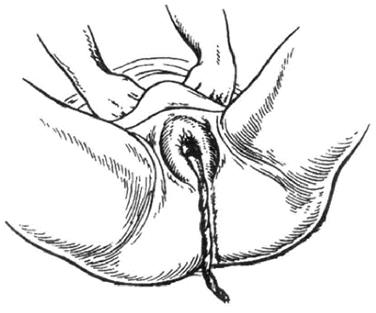
Fig. 131. Henter’s method
Fundal pressure. The fundus is pushed downwards and backwards after placing four fingers behind the fundus and the thumb in front using the uterus as a sort of piston. The pressure must be given only when the uterus becomes hard (Crede’s method) (Fig. 132).
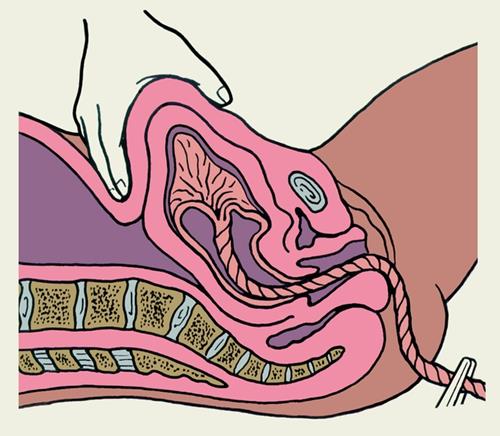
Fig. 132. Crede’s method
After placental expulsion the uterus must be massaged to make it contract which facilitates expulsion of retained clots, if any. Injection of ergometrine 0. 5 mg intramuscularly or Sintocinon 5IU/mL intravenously may be given. Examination of the placenta and membranes is necessary to prevent complications. The placenta is placed on a table and the maternal surface is first inspected by spreading the placenta over the two hands. It is better to examine the placenta convex over the backs of both hands to reproduce its position in the uterus. The maternal surface is covered with grayish deciduas (spongy layer of the decidua basalis). Normally the cotyledon is placed in close approximation and any gap indicates a missing cotyledon. The villi should not be seen free and floating. Abnormal degenerative changes and any morphological abnormalities are to be noted. The membranes and chorion are to be examined carefully for completeness and presence of abnormal vessels indicative of succenturiate lobe. If the membranes are complete, the hole in the membranes becomes round. The chorion leaves deciduas capsularis and bits of deciduas vera. An oval gap in the placenta with torn ends of blood vessels running up to margin of the gap indicates a missing succenturiate lobe. The absence of cotyledon or evidence of a missing succenturiate lobe or evidence of significant (more than 2/3 parts) missing membranes demands exploration of the uterus urgently. Manual examination and obtaining of retained parts should be done with the help of anesthesia.
The cervix of the uterus is inspected by speculum carefully for injuries. The vulva, vagina and perineum are inspected for injuries, to be repaired if any. The episiotomy or perineotomy wound is sutured.
Еarly Postpartum Period
The maternal condition — pulse, blood pressure, behavior of the uterus and any abnormal vaginal bleeding — is to be watched at least for 2 hours after delivery. When fully satisfied that the general condition is good, pulse and blood pressure are steady, the uterus is well contracted and there is no abnormal vaginal bleeding, the patient is sent to the ward.
Self Test
1. Estrogen is able to:
A. activate the receptors for oxytocin in the myometrium and deciduas
B. stimulate uterine contractions
C. decrease uterine tone
D. increase the level of endogenous oxytocin
E. increase the level of prostaglandin
2. The first stage of labor starts with:
A. onset of regular labor pains
B. engaging of the fetal head,
C. rupture of “bag of waters”
D. extension of the head
E. onset of lower abdominal pains
3. The second stage starts with:
A. the full dilatation of the cervix
B. rupture of water membranes
C. engaging of the fetal head
D. extension of the head
E. crowning of the head
4. The third stage of labor begins:
A. after expulsion of the fetus
|
|
|
B. after expulsion of the afterbirth
5. Central separation of placenta is:
A. separation by Schults
B. separation by Duncan
6. An active phase of the first stage of labor takes place:
A. from 4 to 8 cm opening of the cervix
B. from 0 to 4 cm opening of the cervix
C. from 8 cm opening of the cervix.
CHAPTER 15. Preparation of pregnants for labor and delivery. Pain relief in labor
Preliminary preparation of pregnant for birth
Preparation of pregnant for birth should begin from the moment of establishment of diagnosis of pregnancy.
The essence of all measures to be taken is the following:
• Psychoprophylactic or physiopsychoprophylactic preparation;
• Establishment of individual diet and regimen of working activity;
• Acquiring common and special hygienic knowledge to provide health of mother and future child.
Psychoprophylactic preparation of pregnant for birth is a complex of measures including medical physical education, ultraviolet irradiation and special studies.
The method of psychoprophylactic preparation of pregnant for birth is based on the teaching about essence of labor pain, which forms not only due to irritation of the nervous endings on the part of uterus and other genital organs, but also owing to a conditional reflex component related to the influence on the cortex of the central nervous system. Thus, it is acknowledged that a leading role in the origin of pain feeling belongs to the cortex.
The essence of this method consists in the verbal effect on decreasing excitation in subcortical centers and balancing the processes of excitation and inhibition in the cortex.
The purpose of psychoprophylactic preparation is to eliminate fear before delivery and other negative emotions occurring during pregnancy, to give an idea of a labor act as a physiological and painless process, to stir up a new positive feeling connected with forthcoming maternity.
Psychoprophylactic preparation for delivery begins with the first visit of the woman to maternity welfare clinic. A doctor finds out the social and living conditions of pregnant, her attitude towards pregnancy and forthcoming delivery, presence of harmful habits. A woman is acquainted with the rights of pregnant and nursing mothers, and benefits to them. A doctor finds out, whether the woman is in fear of delivery, persuades her of necessity of special preparation for delivery, which helps to avoid the pain feeling. A doctor should try to render a favorable influence on the psyche of pregnant, constantly underlining the fact that delivery is a physiological act and its course to a great extent depends on woman’s preparedness for birth and maternity.
From the 30th week (the beginning of maternity leave), the instruction is conducted especially thoroughly. At good preliminary preparation, it is quite sufficient to have 4-5 lessons, the last one being arranged 6-7 days before birth. At late follow-up, pathological course of pregnancy, burdened obstetric anamnesis, extragenital pathology the number of classes increases up to 6-9; they are conducted individually twice a week. The healthy pregnant are trained in groups of 8–10 persons, which are composed, if possible, of the same emotional type of women.
The first lesson. Pregnant get brief information about the anatomic structure of woman’s genital organs, about uterus as a fetus container and organ of fetus feeding. Information on development of fetus, its position in the uterus, role of placenta, amniotic fluid is also given. The essence of changes in the organism of pregnant providing the physiological course of pregnancy and birth is elucidated.
The second lesson. Pregnant are given an idea of birth as a physiological act, of periods of birth. The features of birth period, subjective feelings of a woman giving birth are explained; the notion of contractions, their duration and regularity is given. The mechanism of effacement and opening of uterus neck, the role of a fetal bladder and amniotic fluid are elucidated.
|
|
|
The third lesson. Pregnant are explained how to behave at appearance of contractions and during the first period of delivery. They are taught to differentiate pain from contractions, in many women the contractions occur quite painlessly. Women are taught special methods to decrease the pain feeling: the correct, even and deep breathing during contractions; slight massage of anterior lateral surfaces of the abdomen on inhalation and exhalation; massage of skin of the lumbar area; pressing by large fingers of skin against two anterosuperior iliac spine; pressing by fists of points corresponding to the inner corners of the Michaelis’ rhombus; counting the number of contractions; relaxation and, if possible, drowsing between the contractions. Pregnant should master well the indicated recommendations and exactly follow them. At the end of the lesson the reasons which can strengthen painful sensation in delivery are explained, e. g. fear, uneasy behaviour, overfilled urinary bladder. It is necessary to underline that these reasons are easily eliminated in delivery by the correct behaviour of woman.
The fourth lesson. An insight into the course of second and third periods of birth, character of feeling of woman giving birth at this time is provided. Rational positions are recommended at the beginning and end of expulsion period, when a woman giving birth have to manifest maximum of physical and psychic efforts, be able to hold breath in order to increase efficiency of bearing down efforts and weaken musculature in the moment of birth of fetus’ head. The emphasis is laid on the fact that duration of the second period of birth depends not only on correct application of methods and techniques, but also on sufficient physical training. It is recommended to train these methods at home until their complete mastering. Information is given on the course and essence of afterbirth period, its duration, character of contractions. Women are taught to behave correctly during the delivery of placenta.
The fifth lesson. As a rule, it is a final lesson which goal is to revise in short and check the material of the previous lessons. It is told about a routine and situation in a maternity hospital, about the rules of asepsis and antisepsis. The information on obligatory and possible medical-diagnostic measures is given (external and vaginal examination, dissection of fetal bladder, intravenous and intramuscular injections, inhalation of oxygen, etc). Their validity and necessity for the normal course and completion of childbirth are explained.
Psychoprophylactic preparation of pregnant to birth is useful to combine with the ultraviolet irradiation (UVI) which improves the functional state of the nervous system, endocrine glands, increases the resistance of organism to infection, is instrumental in normalization of metabolism of vitamins. UVI is carried out according to the method offered by A. A. Lebedev. By 16 weeks of pregnancy 10 sessions of common ultraviolet irradiation of intensity 0. 25–1. 25 biodose are administered, in the pregnancy term of 16–31 weeks — 10 sessions of intensity 1. 25–1. 5 biodose and by 32-40 weeks — 20 sessions of intensity 1. 5 — 2. 5 biodose.
Psychoprophylactic preparation of pregnant for delivery should be combined with physical exercises, which are recommended from the beginning of pregnancy. Systematic physical training promotes the increase of organism resistance to infection, strengthens the nervous system, heartens up, and improves general condition, appetite, sleep, work of cardiovascular, respiratory, gastrointestinal system. Physical exercises strengthen the muscles of the pelvic bottom, front abdominal wall, eliminate the stagnant phenomena in small pelvis and lower extremities, and contribute to the normal course of delivery and postnatal period.
|
|
|
Physical training is conducted more frequently in groups under supervision of instructor or specially trained midwife. After the proper training, the fulfilment of these exercises is allowed at home, in this case the correct fulfilment of exercises is checked up every 10 days.
Physical training is recommended in the morning before the meal or 1–2 hours after breakfast in a well-ventilated apartment, in free clothes not interfering with movements. The duration of training should not exceed 15-20 min. The complex of exercises should not cause fatigue, difficulties of breathing, palpitation, shortness of breath, etc. in pregnant. Jumps, considerable straining effort, jerks should be excluded.
Physical training is recommended only to healthy women, with the physiological course of pregnancy.
Contraindications to physical training:
• acute infectious diseases;
• decompensated diseases of the cardiovascular system;
• illnesses of liver and kidneys;
• complications of pregnancy (gestoses, threat of miscarriage, bleeding during pregnancy).
Except for physical exercise there are other means to be physically fit, such as walks in fresh air, the dosed air-baths, vitamin therapy, rational diet, etc.
Medicinal preparation to delivery
Medicinal preparation for delivery can be done in case of absence of natural readiness of organism for birth to prevent post term pregnancy and anomalies of labor pains and for prophylaxis of hypoxia of fetus during delivery.
A complex of signs, which occurrence indicates that delivery will begin in the nearest time, characterizes readiness of organism for delivery.
By clinical methods of research such signs of organism readiness to birth are determined as:
• mammarian test
• oxytocin test
• cytological research of vaginal smear
• determination of maturity of the uterus cervix.
The mammarian test. It is the most simple and accessible test which a doctor can begin with. By massaging motions of fingers, as at straining milk, one begins to irritate a nipple and areola, palpating uterus by the other hand. The irritation is produced during 3 minutes. If in this period the contraction of uterus (rise of its tone) takes place, the test is considered positive. The irritation of receptors of nipple, nipple channel and cistern results in reflex of milk delivery, which hormonal component is the secretion of oxytocin from neurohypophysis. Oxytocin causes contraction of uterus. The test is positive, if myometrium has sufficient excitability, and the dominant higher nervous-reflex links are found in a state of readiness to birth.
The oxytocin test. Its mechanism is similar to that of the mammarian test. Offered first by Smith (1953), it is now performed in the Eddie modification. In 100 ml of 5% solution of glucose or physiological solution of sodium chloride 0. 2 ml (1 IU) oxytocin are mixed. It turns out that 1 ml solution contains 0. 01 IU oxytocin. In syringe 5 ml solution (0. 05 IU) are taken and slowly introduced intravenously at a speed of 1 ml per minute, registering contractions of uterus. Registration of uterus contraction can be checked by palpation, hysterography, cardiotocography or ultrasonography. The test is positive if uterus contracts in the first three minutes of introducing preparation, in other words, at doses of oxytocin from 0. 01 to 0. 03 IU. At large doses the test is considered negative.
Cytological research of vaginal smear. The test is conducted before vaginal research. Vagina is revealed in specula and by a grooved probe or pincers a vaginal smear is taken from the lateral side of the vagina wall on the border of the upper and middle third (the most sensible place to hormonal changes). The material is put on clean glass by a thin layer and fixed in the Nikiforov’s mixture (a 50% mixture of alcohol and ether) during 15 minutes or in air for 20 minutes, then it is dyed by Romanovsky (by methylene-blue, azur-eosin) and observe under microscope at small magnification, and then at large magnification. According to classification by Ya. Zhidovski (1960) four types of cytological smears are distinguished:
The I type of smear — navicular, or “late term of pregnancy”. In the smear scaphoid and intermediate cells prevail in ratio 3: 1 as accumulations, their cytoplasm being high-contrast basophilic; mucus and leucocytes are not present. The karyopyknotic index (KPI) is not more than 1–3 %. KPI is a percent correlation of superficial cells with pyknotic nuclei (that is with a diameter less than 6 µ) to the cells with non-pyknotic nuclie (more than 6 µ in diameter). It characterizes the estrogenic saturation of organism. KPI 1-3 % means that the estrogenic saturation of organism is low, delivery may be expected not earlier than in 10 days.
|
|
|
The II type of smear — “shortly before birth”. In the smear less scaphoid but more intermediate and superficial cells are determined (the ratio is 1: 1). Accumulations disintegrate, cells lie in a more isolated way, mucus and leucocytes are not present. KPI is 4–8%. Delivery should be expected in 4–8 days.
The III type of smear — “term of birth”. In the smear the scaphoid cells are almost absent, the intermediate and superficial ones prevail. Mucus and leucocytes appear. KPI is 15–20 %. Delivery may be expected in 1–5 days.
The IV type of smear — “undoubted term of birth”. In the smear the isolated superficial cells are determined, dim painted, without clear scopes. A lot of leucocytes and mucus are present. KPI is up to 40%. Delivery can start during the nearest day.
Evaluation of maturity of the uterus cervix
To estimate the degree of “maturity” of uterine cervix before birth a simplified scale offered by E. H. Bishop is used (Table 9).
At vaginal research of the uterine cervix its consistency, length of vaginal part, degree of dilatation of cervical channel, location in the small pelvis in relation to the axis of pelvis are determined by palpation. Every sign is estimated from 0 to 2 points.
Maturity of neck of uterus is estimated according to the sum of points:
0-2 points — cervix is immature;
2–4 points — cervix is not sufficiently matured;
5–8 points — cervix is matured.
Table 9
Scale of estimation of “maturity” degree of the uterine cervix according to E. H. Bishop
| Sign | 0 point | 1 point | 2 points |
| Consistency of cervix of uterus | Dense | It is softened, but in the area of internal pharynx the ring of compression is palpated | Soft |
| Length of cervix of the uterus | More than 2 cm | 1 — 2 cm | Less than 1 cm or smoothed out |
| Permeability of cervical canal | External os is closed, or allows the dome of finger | The canal is passable for 1 finger, but there is compression in the area of internal pharynx | Cervical canal is dilated for 1–2 fingers (2-4 cm) |
| Position of cervix of the uterus | It is deviated backwards from the pelvic axis | It is deviated forwards from the axis of pelvis | It is located according to the pelvic axis |
Modified Bishop scale is mostly useful now-a-days in foreign countries (Fig. 133)
Fig. 133. Modified Bishop scale.
Anaesthetizing Labor (Labor Pain Relief)
There are several different forms of anesthesia administered for childbirth. They may be used independently or in conjunction with one another. Some of the most commonly administered anesthetics include:
Local anesthesia: infiltration of local anesthetics.
Sedation: administration of narcotics or tranquilizers.
Regional anesthesia: pudendal block (injections of local anesthetics to numb vaginal area) in preparation for delivery.
Epidural anesthesia: a local anesthetic is inserted into the epidural space of the spinal cord through the epidural catheter. An advantage of the epidural is that it allows most women to fully participate in the birth experience (continue to feel touch and pressure) while relieving most, if not all, of the pains of labor. In most cases, the anesthetist will start the epidural when cervical dilation is 4 to 5 centimeters.
Spinal anesthesia: anesthetic is similar to an epidural, but because it is administered with a needle into the spinal canal, its effects are felt much faster. Spinal anesthetics may be used for delivery by cesarean section or when the forceps use is indicated.
Epidurals or spinals cannot be used if the patient:
- Uses blood thinners or has a bleeding tendency.
- Is hemorrhaging or in shock.
- Has an infection in the back or the blood.
- Has an unusual anatomic condition or spinal abnormality. Additionally, if time is of the essence.
General anesthesia:
General anesthesia is administered by giving anesthetic drugs intravenously and having the patient breathe anesthetic gases. A general anesthetic may be necessary if complications arise during delivery. General anesthetics can be administered quickly, so they're considered the best choice when time is of the essence. Also, general anesthesia enables the uterus to relax if it becomes necessary.
Indications for anesthesia in labor:
· Marked obesity
· Obstetric complications with potential for operative delivery (eg, placenta previa, high order multiple gestation)
· Severe preeclampsia
· Bleeding disorders (eg, thrombocytopenia)
· Use of anticoagulants
· Severe edema, trauma, surgery, or anatomical abnormalities of the face, neck, or spine
· Abnormal dentition, small mandible, or difficulty opening mouth
· Extremely short stature, short neck, or arthritis of the neck
· Goiter
· Prior history of anesthesia complications, such as malignant hyperthermia
· Cardiovascular, neurological, or respiratory disease
· Hyperreflexia in parturients with a high spinal cord lesion (prevention or treatment)
|
|
|