 |
Fetal heart rate pattern classification and interpretation
|
|
|
|
Fetal heart rate pattern classification and interpretation
| Category | Interpretation | Features |
| I Normal | Tracings in this category are strongly predictive of normal acid-base status at the time of observation | Baseline rate 110 to 160 beats per minute • Baseline variability moderate • Late or variable decelerations absent • Early decelerations present or absent |
| II Indeterminate | Tracings in this category are not predictive of abnormal acid-base status, however there are insuffi - cient data to classify them as either category I or category III. | All tracings not categorized as category I or III and may represent many tracings that are encountered in everyday clinical practice. Examples: • Minimal variability • Absent variability without recurrent decelerations • Marked variability • Absence of induced accelerations after fetal stimulation • Recurrent variable decelerations with minimal or moderate variability • Prolonged deceleration • Recurrent late decelerations with moderate variability • Variable decelerations with “slow return to baseline”, “overshoots” or “shoulders” |
| III Abnormal | Tracings in this category are predictive of abnormal acid-base status at the time of observation. | Absent variability and any of the following: - Recurrent late decelerations - Recurrent variable decelerations - Bradycardia • Sinusoidal pattern |
A – Accelerations
Accelerations are periodic, transient increases in FHR, defined as an increase in FHR > 15 bpm for more than 15 seconds. When accelerations are present, the CTG is said to be reactive. Accelerations are often associated with fetal activity and are considered an indication that the fetus is healthy. (Fig. 78)
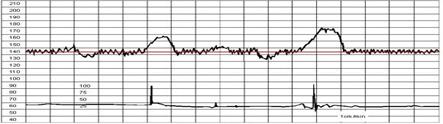
Fig. 78. Accelerations.
Based on visual assessment, an acceleration is defined as an abrupt increase of at least 15 beats per minute in fetal heart rate above the baseline. Onset to peak is less than 30 seconds and duration is equal to or more than 15 seconds and less than two minutes from onset to return to baseline. The duration of an acceleration is defined as the time from the initial change in FHR from the baseline to the return of the FHR to the baseline. At 32 weeks of gestation and beyond, acceleration has a peak of 15 beats per min or more above baseline, with a duration of 15 sec or more but less than 2 min. In pregnancies less than 32 weeks gestation, has a peak of 10 beats per minute or more above baseline which, with a duration of 10 seconds or more but less than 2 min. An acceleration is classified as prolonged if the duration is 2 minutes or more but less than 10 minutes. If acceleration lasts 10 mins or longer, it is a baseline change.
Accelerations of the FHR may be periodic (that is, occurring in relation to a contraction) or episodic (no association with a contraction). Most are episodic.
These episodic accelerations are generally in response to fetal movement, with a need for increased perfusion, and therefore transiently increased sympathetic tone, or due to fetal stimulation, such as scalp stimulation with a vaginal exam, abdominal palpation, or vibroacoustic stimulation.
|
|
|
Periodic accelerations are those associated with uterine contractions and may be due either to fetal stimulation (particularly in breech presentation) or due to mild cord compression (that is, compression of the umbilical vein only).
FHR accelerations and good (moderate) variability are closely associated and sometimes may be visually indistinguishable, though both are reflective of a well-oxygenated fetus.
The presence of accelerations forms the basis of the nonstress test (NST). A NST is said to be reactive when there are at least two accelerations in a 20 minute period, along with moderate variability and no decelerations.
D – Decelerations
A deceleration is a loss of heart rate of > 15 bpm for > 15 s. Decelerations are periodic, transient decreases in FHR, usually associated with uterine contractions. They can be subdivided into four main types by their shape and timing in relation to uterine contractions. Uterine contractions must be monitored adequately in order for a deceleration to be correctly classified.
Decelerations may be:
• Early (Dip I)
• Late (Dip II)
• Variable
• Prolonged
Early decelerations (Fig. 79)
Early decelerations tend to occur with each contraction and are uniform in shape. Early FHR decelerations appear as a mirror image of the uterine contraction trace. The onset of the deceleration occurs at the onset of the contraction and the baseline FHR recovers by the end of the contraction. The FHR usually does not fall by more than 40 bpm during an early deceleration. Early decelerations are caused by compression of the fetal head during a contraction. They are often relieved by changing maternal posture and are a normal finding in the second stage of labor. They are not associated with a poor fetal outcome.
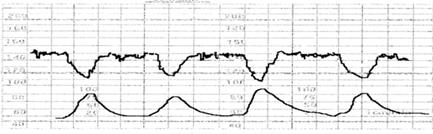
Рис. 79 Dip I – Early decelerations.
Thus, early deceleration has the characteristic mirror image of the contraction. Although these decelerations are not associated with fetal distress and thus are reassuring, they must be carefully differentiated from the other, nonreassuring decelerations.
Late decelerations (Fig. 80)
Late decelerations are associated with uteroplacental insufficiency and are provoked by uterine contractions. Any decrease in uterine blood flow or placental dysfunction can cause late decelerations. Maternal hypotension and uterine hyperstimulation may decrease uterine blood flow. Postdate gestation, preeclampsia, chronic hypertension and diabetes mellitus are among the causes of placental dysfunction. Other maternal conditions such as acidosis and hypovolemia associated with diabetic ketoacidosis may lead to a decrease in uterine blood flow, late decelerations and decreased baseline variability.
A late deceleration is a symmetric fall in the fetal heart rate, beginning at or after the peak of the uterine contraction and returning to baseline only after the contraction has ended (Figure 80). The descent and return are gradual and smooth. Regardless of the depth of the deceleration, all late decelerations are considered potentially ominous. A pattern of persistent late decelerations is nonreassuring, and further evaluation of the fetal pH is indicated. Persistent late decelerations associated with decreased beat-to-beat variability is an ominous pattern. (Fig 81)
|
|
|
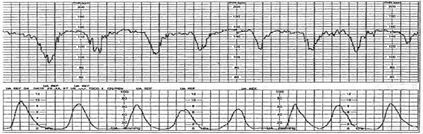
Fig. 80. Dip II - Late decelerations

Fig. 81. Late deceleration with loss of variability. This is an ominous pattern, and immediate delivery is indicated.
Variable decelerations (Fig. 82)
Variable decelerations are shown by an acute fall in the FHR with a rapid downslope and a variable recovery phase. They are characteristically variable in duration, intensity and timing. They resemble the letter “U, ” “V” or “W” and may not bear a constant relationship to uterine contractions. They are the most commonly encountered patterns during labor and occur frequently in patients who have experienced premature rupture of membranes and decreased amniotic fluid volume. Variable decelerations are caused by compression of the umbilical cord. Pressure on the cord initially occludes the umbilical vein, which results in an acceleration (the shoulder of the deceleration) and indicates a healthy response. This is followed by occlusion of the umbilical artery, which results in the sharp downslope. Finally, the recovery phase is due to the relief of the compression and the sharp return to the baseline, which may be followed by another healthy brief acceleration or shoulder
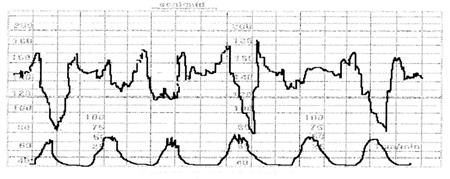
Fig. 82. Variable decelerations.
Variable decelerations may be classified according to their depth and duration as mild, when the depth is above 80 bpm and the duration is less than 30 seconds; moderate, when the depth is between 70 and 80 bpm and the duration is between 30 and 60 seconds; and severe, when the depth is below 70 bpm and the duration is longer than 60 seconds. A persistent variable deceleration pattern, if not corrected, may lead to acidosis and fetal distress and therefore is suspicious (nonreassuring). Suspicious variable decelerations associated with the loss of beat-to-beat variability correlate substantially with fetal acidosis and therefore represent an ominous pattern.
Prolonged decelerations/ bradycardia (Fig. 83., 84).
A deceleration with a reduction in FHR of greater than 30 bpm that lasts for at least 2 minutes is termed a prolonged deceleration. Prolonged decelerations last longer than two minutes, but less than 10 minutes. They are caused by a decrease in oxygen transfer to the fetus so can arise as a consequence of a wide variety of disorders including:
• Maternal hypotension
• Umbilical cord compression
• Uterine hyper tonicity
Thus, more often it associated with hypoxia. Prolonged decelerations are more likely to be associated with cord compression, profound maternal hypotension or hypoxemia, tetanic uterine contractions, or prolonged head compression associated with the second stage of labor. A FHR above 100bpm with good variability is tolerable, but a prolonged deceleration below 100 beats/min calls for immediate efforts at resolution and a drop below 60 bpm becomes an obstetric emergency since it is almost always associated with fetal hypoxia.
A prolonged deceleration that is sustained for 10 minutes or more is a baseline change.

Fig 83. Prolonged deceleration of fetal heart rate (FHR) with slow recovery.

Fig. 84. Prolonged deceleration of fetal heart rate (FHR) without recovery.
|
|
|


