 |
Ultrasonography in the second trimester
|
|
|
|
Ultrasonography in the second trimester
At the 2nd sonographic screening (at 18-21 weeks of pregnancy) the US exam is
focuses on the anatomical features of the fetus to exclude congenital malformations, the presence of a later manifestation of chromosomal pathology, assess the growth of the fetus, evaluate the amount of amniotic fluid, localization and attachment of the placenta; and assess the length of the cervix as prognostication of preterm labor. The condition of myometrium and adnexa is also controlled.
Indications for selective (if indicated) ultrasound in the second trimester of pregnancy:
1. The discrepancy between the estimated gestational term and size of the uterus (suspected intrauterine growth restriction (IUGR), undeveloping pregnancy, to avoid oligohydramnios, polyhydramnios, multiple pregnancy, etc. );
2. Ultrasonic support of multiple pregnancy, immune incompatibility, invasive techniques of prenatal diagnosis (amniocentesis, placentocentesis, cordocentesis), intrauterine medicinal- diagnostic manipulations (intrauterine blood transfusion to the fetus, in utero puncture of the fetus organs and cavities) and intrauterine operations on fetus;
3. The presence of vaginal bleeding;
4. The presence of tumor-like formations in the pelvic area.
Ultrasound examinations during the third trimester
Ultrasound in the third trimester
The purpose of ultrasound in the third trimester (30-34 weeks gestation) assessment is not so much anatomical, many of the functional characteristics of the fetus to ascertain the capacity of key life-support systems (placenta, heart, feto-placental hemodynamics) for elaboration of further tactics of management of pregnancy and childbirth. During this period, the most active use of ultrasonic methods based on the Doppler effect (Doppler investigation of vessels of fetoplacental uniot and cardiotocography).
DOPPLER IN OBSTETRICS
The most important system, supporting the livelihoods of the fetus, which determines the development of tissues and organs, and directly affect the rate of intrauterine growth - fetal circulation system, directly depends on maternal hemodynamic. Therefore, by assessing the reserve capacity of the fetus, obstetricians must always carry out a comprehensive assessment of the utero-placental-fetal blood flow.
It is well known that during pregnancy, utero-placental blood flow in the first and early second trimester is converted from highly resistant to lower resistant vascular system by 2 wave of invasion of trophoblast into spiral arteries of the uterine wall (upto the ends of radial arteries). At this time musculo- elastic elements of their wall is replacement with a mixture of fibrinoid and connective tissue. Thus, small spiral arteries are replaced with larger vascular channels (Fig. 49).
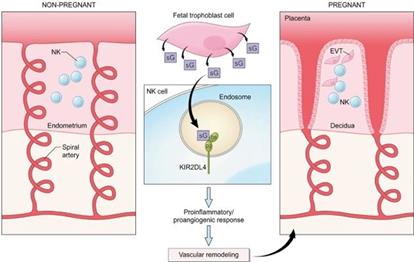
Fig. 49. The processes of vascular remodeling in the uterine artery.
Сhanges in the blood vessels of the fetus to optimize the it’s the circulatory system is a reflection of this process.
|
|
|
Doppler indicated for:
1. Patients with history of low baby weight at birth, and prenatal death.
2. Patients with extragenital disease; cardiovascular, diabetes mellitus, kidney disease, etc.
3. Patients with hypertensive disorders in pregnancy.
4. Patients with intrauterine growth retardation (IUGR) in pregnancy
5. Patients with multiple gestation.
6. Patients with high risk of developing anemia in the fetus.
7. In case of use inhibitors of prostaglandins (to avoid premature closure of the
ductus arteriosus) in pregnancy
8. In case of doubtful or negative result of the evaluation of biophysical profile
profile (BPP)
9. Patients with impaired reactivity of cardiac activity of the fetus by antenatal
cardiotocography (CTG)
Doppler should not be conducted during periods of motor activity of the fetus. In the third trimester the investigation should be made in lateral position of mother, to prevent the development of inferior Vena cava syndrome.
CHAPTER 8. MATERNAL PELVIS AS A PASSAGE, FETUS AS A PASSENGER IN LABOR
Maternal Pelvis
Pelvis is of great significance in obstetrical practice. It forms a birth canal during labor. A female pelvis differs from a male one: female bones are thinner and smoother. A female pelvis is shorter and wider than a male one. (Fig 50).
Fig. 50. Female pelvis.
The cavity of female pelvis looks like a cylinder, and of a male one is crater-like. The pelvis of an adult woman consists of 4 bones: two innominate bones, sacrum and coccyx. These are united together by four joints: two sacroiliac joints, a sacrococcygeal joint and symphysis pubis. (Fig. 51).

Fig. 51. Joint of female pelvis.
Pelvis is anatomically divided into a true pelvis and a false pelvis, the boundary line being the brim of the pelvis. The bony landmarks on the brim of the pelvis from anterior to posterior on each side are the upper border of symphysis pubis, pubic crest, pubic tubercle, pectineal line, iliopubic eminence, iliopectineal line, sacroiliac articulation, anterior border of the sacral promontory.
False pelvis
The false pelvis is much wider than the true pelvis. It is bounded laterally by the large iliac bones, posteriorly — by the last lumbar vertebrae, and anteriorly — by the lower portion of the abdominal wall. It is of little obstetric significance except for the fact that its measurements can to a certain extent predict the size and configuration of the true pelvis. The most important diameters are the following:
• interspinous diameter: 25-26 cm — it is the distance between two anterosuperior iliac spines;
• intercristal diameter: 28-29 cm — it is the distance between the most widely separated points on the outer border of the iliac crests;
• intertrochanteric diameter: 31-32 cm — it is the distance between the trochanters of both sides;
• external conjugate (Baudelocque’s diameter): 20-21 cm — it is the distance between the tip of the 5th lumbar vertebra and the upper border of the anterior surface of the symphysis pubis.
All those diameters are taken by external pelvimetry with the help of pelvimeter or callipers (obstetrical examination).
True pelvis
This part of pelvis is the most important for obstetricians, as it forms the canal through which the fetus passes during labor. Its smallest anterior part is formed by symphysis pubis and measures about 4 cm; a deeper posterior part is composed of sacrum and coccyx and makes up about 11. 5 cm.
|
|
|
Obstetrically it is divided into 4 planes:
• a plane of inlet
• cavity
• obstetrical outlet
• anatomical outlet (Fig. 52, 53).
Fig. 52. Pelvic planes.
Fig. 53. Pelvic planes, side view.
All those are imaginary flat surfaces, but not mathematical ones.
I. Inlet — the circumference of the inlet is formed by the superior margin of the symphysis pubis (anteriorly), pectineal line (laterally), sacral promontory (posteriorly).
Shape: it is normally more oval than round with anteroposterior diameter being the shortest.
Inclination: in the erect posture the pelvis is tilted forwards. Thus, the plane of the inlet makes an angle of about 55 degrees with the horizontal and is called the angle of inclination. Little inclination facilitates the fetus head engagement passing through the pelvis.
Diameters: all measurements of the diameters are approximate. They are the following:
• Antero-posterior diameter (syn: true conjugate, obstetric conjugate, “conjugata vera”). It is the distance between the midpoint of the sacral promontory and the inner margin of the symphysis pubis. It measures about 11 cm. Its measurement is determined by subtracting 2. 0 — 1. 5 cm from the diagonal conjugate. Diagonal conjugate is the distance between the lower border of the symphysis pubis and the midpoint of the sacral promontory. It measures more than 12 cm. The distance between the midpoint of the sacral promontory and the outer margin of the symphysis pubis is called anatomical conjugate and makes up 11. 5 cm.
• Transverse diameter: it is the distance between the two farthest points of the pelvic brim over the iliopectinal lines. It measures 13 — 13. 5 cm. The diameter divides the brim into anterior and posterior segments.
• Oblique diameters: There are two oblique diameters — right and left. Each one extends from one sacroiliac joint to the opposite iliopubic eminence and measures 12-12. 5 cm. The right or left diameter denotes the sacroiliac joint from which it starts.
II. Cavity. It is a segment of pelvis bounded above by the inlet and below by the plane of the obstetrical outlet. This plane extends from the midpoint of the symhysis pubis to the junction of the second and third sacral vertebrae, laterally — between two acetabular surfaces. It is called the plane of the greatest pelvic dimensions. This plane presents the continuous bony ring of the pelvis.
Shape: It is almost round.
Diameters:
• Antero-posterior diameter: 12 cm. It measures from the midpoint of the posterior surface of the symphysis pubis to the junction of the second and third sacral vertebrae.
• Transverse diameter: 12 cm. It is the distance between the furthest points of internal surfaces of acetabulum (cotyloid cavities).
Ш. Obstetrical outlet. It is a segment of pelvis bounded above by the plane of the greatest pelvic dimensions and below — by the anatomical outlet. Its anterior wall is formed by the pubic arch, its lateral walls are formed by ischial bones and the posterior wall includes the tip of the sacrum. It is the plane of the least dimensions or narrow pelvic plane. This plane extends anteriorly from the lower border of the symphysis pubis, laterally to the tip of ischial spines and posteriorly to the tip of the 5th sacral vertebra.
Shape: it is anteroposterior oval.
Diameters:
• Antero-posterior diameter: 11 cm. It extends from the inferior border of the symhysis pubis to the tip of the sacrum (or joint of the sacrum and coccyx).
• Transverse diameter (syn.: bispinous) equals to 10. 5 cm. It is the distance between the tips of two ischial spines (the narrowest diameter of the pelvis).
|
|
|
IV. Anatomical outlet. It is bounded in front by the lower border of the symhysis pubis, laterally by the ischiopubic rami, ischial tuberosity and sacrotuberous ligament and posteriorly by the apex of coccyx. Thus, it consists of two triangular planes with a common base formed by a line joining the ischial tuberosities. The apex of the anterior triangle is formed by the inferior border of the pubic arch and that of the posterior triangle — by the apex of coccyx. The plane is formed by a line joining the lower border of symphysis pubis to the apex of coccyx.
Shape: It is diamond-shaped.
Diameters:
• Antero-posterior diameter. It extends from the lower border of the symphysis pubis to the apex of coccyx. It measures 11. 5 cm with the coccyx pushed back by the head when passing through the plane during labor. In nulliparous its measurement will be 2. 5 cm less (9 — 9. 5 cm).
• Transverse diameter (syn.: intertuberous): 11 cm. It extends between the inner borders of ischial tuberosities.
Pelvic axis. It is formed by joining the axis of inlet, cavity and outlet. It is uniformly curved with the convexity fitting the concavity of the sacrum. The curve bisecting the anteroposterior diameters of the inlet cavity and outlet is called the pelvic axis. It is through this axis that the fetus negotiates the pelvis. Its direction is first downwards and backwards up to the level of ischial spines and then directed abruptly forwards.
Pelvic angle
The ratio of the pelvic plane of inlet to the horizontal plane is called the pelvic angle (inclination pelvis). Normally it is about 55-60 degrees. When the patient is in horizontal position (lying on the back) the angle is about 30 degrees.
Fetal Skull
The head of a mature fetus is termed the fetal skull.
The study of the fetal skull is of great importance. The fetal skull is to some extent compressible, and made mainly of thin pliable flat bones forming the vault, and incompressible bones are at the base of the skull.
The skull is divided into several zones of obstetrical importance. They are the following:
• Vertex. It is a quadrangular area bounded anteriorly by the bregma and coronal sutures, behind — by the lambdoid sutures, and laterally — by lines passing through the parietal eminences.
• Brow. It is an area bounded on one side by the anterior fontanelle and coronal sutures and on the other side — by the root of the nose and supraorbital ridges of either side.
• Face. It is an area bounded on one side by the root of the nose and supraorbital ridges and on the other — by junction of the floor of the mouth with neck. (Fig. 54).
Fig. 54. Fetal skull, view from above: BiP –biparietal diameter; BiT- bitemporal diameter.
Sinciput is the area lying in front of the anterior fontanelle and corresponds to the area of the brow and the occiput is limited to the occipital bone.
Flat bones of the vault are united by non-ossified membranes attached to the margins of the bones. These are called sutures and fontanelles.
The following sutures are of most significance in obstetrical practice.
• The sagittal (longitudinal) suture — between two parietal bones. Anteriorly it is bounded by the large fontanelle, and posteriorly — by the small fontanelle.
• The frontal suture is the junction of the two frontal bones. The direction is the same as of the sagittal one.
• The coronal sutures lie between the parietal and frontal bones on either side. Its direction is perpendicular to the sagittal and frontal sutures.
• The lambdoid suture lies between the occipital and parietal bones.
|
|
|
Fontanelle is a wide gap in a suture line, free of ossification. Fontanelle can facilitate the molding of the head during labor.
The following fontanelles are of great importance in obstetrical practice:
• Anterior (or large) fontanelle. It is formed by joining the four sutures: frontal, sagittal and two coronal in the midplane. It is diamond-shaped. In mature fetus its diameter is about 30 mm.
• Posterior (or small) fontanelle. It is a triangular soft area, formed by junction of three sutures: the sagittal suture (anteriorly), and lambdoid suture (laterally on the left and right sides).
Diameters of the fetal skull
The following diameters are of great importance in obstetrical practice (Picture 23):
• The suboccipitobregmatic diameter, called a small oblique diameter. It is the distance between the anterior angle of the large fontanelle and the lowest posterior point of the occiput. Usually it is about 9. 5 cm; its circumference is about 32 cm.
• The suboccipitofrontal diameter, which is measured from the anterior margin of the haired part of the forehead to the lowest posterior point of the occiput. Usually it is about 10 cm, circumference is about 33 cm.
• The occipitomental diameter, called a large oblique diameter. It is measured from the external occipital protuberance to the most prominent point of the chin. It is the largest diameter of the head, about 13 cm, and 35-36 cm in circumference.
• The occipitofrontal diameter — from the midpoint of the frontal bone (glabella) to the external occipital prominence. It is about 12 cm, and about 34 cm in circumference.
• The vertical diameter — between the vertex and sublingual area, is about 9. 5-10 cm. The head circumference at this level is 33 cm.
• The biparietal diameter (called a large transverse diameter) — it is the distance between the two parietal eminences; it makes up 9. 5 cm.
• The bitemporal diameter (a small transverse diameter) — is a distance between the two extreme points of the coronal suture; it makes up 8 cm.
• The most important diameters of the fetal body are:
• The biacromial diameter — between the extreme points of the shoulder girdle — equals to 12 — 12. 5 cm, the circumference is 35 cm;
• - The basiliac diameter — between the two most remote points of the iliac crests- makes up 9 — 9. 5 cm, the circumference is 28 cm. (Fig. 55)
Fig. 55. Fetal skull, side view. O. F. -occipito-frontal diameter; O. M. - occipito-mental diameter
Self Test
1. Which of the following is the borderline between the false and true pelvis?
A. iliac bone
B. brim of the pelvis, promontory
C. two sacroiliac joints
2. The interspinal diameter is the diameter of
A. the pelvic inlet
B. the pelvic outlet
C. the pelvic cavity
3. The interspinal diameter is normally about
A. 26-27 cm
B. 25-26 cm
C. 24-25 cm
D. 27-28 cm
4. The intercristal diameter is about
A. 25-26 cm
B. 26-27 cm
C. 27-28 cm
D. 30-32 cm
5. Normal sizes of the false pelvis are:
A. 25-28-30-17
B. 25-28-30-21
C. 25-28-33-13
6. Identify the diameters of the fetul skull, which have the same sizes:
A. small oblique and occipitofrontal diameter
B. occipitofrontal and vertical diameter
C. suboccipitobregmatic and vertical diameter
D. suboccipitofrontal and a large oblique diameter
7. The suboccipitofrontal diameter is about:
A. 8 cm
B. 9. 25 cm
C. 10 cm
D. 13. 5 cm
8. The pelvic angle is about:
A. 45-50°
B. 55-60°
C. 65-70°
D. 40-45°
9. The largest diameter of pelvic planes is:
A. transverse diameter of the pelvic inlet
B. anteroposterior diameter of the pelvic cavity
C. transverse diameter of the anatomical outlet
D. oblique diameter of the pelvic inlet
10. A large oblique diameter is measured from:
A. the external occipital protuberance to the most prominent point of the chin
B. the occiput to the forehead
C. the glabella to the external occipital protuberance
D. the anterior angle of the large fontanelle to the lowest point of the occiput
11. The biparietal diameter is about:
A. 13 cm
B. 12 cm
C. 11 cm
D. 10 cm
12. The biacromial diameter is about:
A. 9 cm
B. 10 cm
C. 11 cm
D. 12 cm
Chapter 9. Physiological changes in maternal organism during pregnancy
Pregnancy is a state of a long physical adaptation, which is necessary for satisfying the needs of growing fetus, and for providing constancy of environment, in which the fetus grows. The degree of this adaptation exceeds the needs of fetus, as a whole, so there are considerable reserves which allow enduring the periods of stress or deprivations without any essential changes of the fetus environment. Each of the systems of mother’s organism undergoes changes.
|
|
|
The Endocrine system
The endocrine system plays an extremely important role in the origin and development of pregnancy.
The changes in all endocrine glands occur with the beginning of pregnancy.
A new endocrine gland — a yellow body of pregnancy- begins to function in one of the ovaries. It exists and functions in the organism during the first 3-4 months of pregnancy. The hormone of the yellow body — progesterone — promotes the implantation of the fertilized ovum in the mucous membrane of uterus, decreases its excitability and favours the development of pregnancy.
Progesterone produces a protective effect on the fertilized ovum and uterus. The transmission of the nervous excitement from one muscular fiber to another slows down under progesterone influence, as a result the activity of neuromuscular apparatus of the uterus decreases. It makes for the further growth of the uterus during pregnancy and development of glandular tissues of mammary glands. The level of progesterone in the first weeks of pregnancy makes up 10–30 ng/ml, increasing from the 7th week of pregnancy.
A yellow body gradually regresses from 10–12 weeks of pregnancy, stopping the function fully to 16 weeks.
At this time a new endocrine gland appears — placenta, which carries out communication of the fetus with the organism of mother. The placenta produces a number of hormones, such as gonadotrophins, progesterone, estrogens and others.
Chorionic gonadotrophin promotes the progress of pregnancy, affects the development of adrenal glands and gonads of the fetus, contributes to the processes of exchange of steroids in placenta.
Chorionic gonadotrophin starts to be determined on the 3rd week of pregnancy. On the 5th week its level in urine makes up 2, 500–5, 000 mIU/ml, on the 7th week rises to 80, 000–100, 000 mIU/ml. At term of 12-13 weeks the maintenance of chorionic gonadotrophin decreases to 10, 000–20, 000 ME/l and remains at this level to the end of pregnancy.
|
|
|


