 |
Try to predict the right answers for the questions:
|
|
|
|
1. Who examines the patient?
o nurse
o doctor
o doctor assistant
2. What is the purpose of asking the patient name and birthdate?
o to identify the patient’s diagnosis
o to identify the patient’s background
o to identify the patient’s personality
3. How does the nurse teach the patient?
o gives the information about follow-up appointment, explains the causes of disease
o gives the information about drug taking and equipment usage, explains the impact of medications, suppliers with supporting information
o explains what vital signs are, prescribes medicines
4. How long should a patient take the antibiotics?
o 7-10 days
o 20-30 days
o 1-3 days
27. Watch the video ‘Taking a Patient's History (Nurse/Patient)’ and check your predictions:
https://www.youtube.com/watch?v=NW-ZRo6GJnA
28. Watch the video once more and fill in the chart:
| Data | |
| Name, birthdate | |
| Chief complaint | |
| Overall patient’s state | |
| Presenting symptoms, complaints | |
| Medications | |
| Smoking | |
| Vital signs (rates) | |
| Follow-up visit | |
| Administrations |
29. Refer the obtained information to the necessary section of Case History:
| Section | Data |
| Identification and demographics | |
| Chief complaints | |
| History of the present illness | |
| Past medical history | |
| Review of systems | |
| Family history | |
| Social history | |
| Medications | |
| Allergies |
Reading

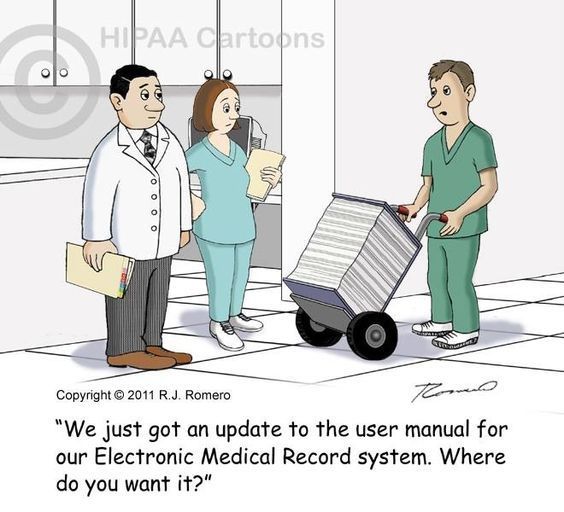
30. Explain the term ‘ medical record ’.
Read the text and choose the sentences that clarify the title of the text.
Medical Record

The terms medical record (health record, medical chart) is used to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. The medical record includes a variety of types of "notes"(admission notes, on-service notes, progress notes (SOAP notes), preoperative notes, operative notes, postoperative notes, procedure notes, delivery notes, postpartum notes, and discharge notes) entered over time by health care professionals, recording observations and administration of drugs and therapies, orders for the administration of drugs and therapies, test results, x-rays, reports, etc. The maintenance of complete and accurate medical records is a requirement of health care providers and is generally enforced as a licensing or certification prerequisite.
The information contained in the medical record allows health care providers to determine the patient's medical history and provide informed care. The medical record serves as the central repository for planning patient care and documenting communication among patient and health care provider and professionals contributing to the patient's care. An increasing purpose of the medical record is to ensure documentation of compliance with institutional, professional or governmental regulation.
|
|
|
Medical records have traditionally been compiled and maintained by health care providers, but advances in online data storage have led to the development of personal health records (PHR) that are maintained by patients themselves, often on third-party websites. This concept is supported by US national health administration entities and by AHIMA, the American Health Information Management Association.
Health information technology (HIT) is "the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making." Health information technology components:
Electronic Health Record (EHR) - An EHR contains a patient's comprehensive medical history, and may include records from multiple providers.
Electronic Medical Record (EMR) - An EMR contains the standard medical and clinical data gathered in one's provider’s office.
Personal Health Record (PHR) - A PHR is a patient's medical history that is maintained privately, for personal use.
Health Information Exchange (HIE) - Health Information Exchange allows health care professionals and patients to appropriately access and securely share a patient’s vital medical information electronically.
Grammar (Revision)
Perfect Active & Passive
32. Translate the sentences into Russian paying your attention to Perfect Active and Perfect Passive:
1.After all of the important history questions have been asked, a focused physical exam is usually done. 2. Computer-assisted history taking systems have been available since the 1960s. 3. For example, patients may be more likely to report that they have engaged in unhealthy lifestyle behaviors. 4. Medical records have traditionally been compiled and maintained by health care providers, but advances in online data storage have led to the development of personal health records. 5. Medical history gives the clinician a feel for what has happened before to the patient. 6. History of the present illness is a detailed exploration of the symptoms the patient is experiencing that have caused the patient to seek medical attention. 7. The United States and the EU have imposed mandatory medical data breach notifications. 8. Every clinical procedure conducted is started because some decision had been made. 9. When new patients enter the typical office, they are greeted, seated comfortably, handed a clip board to which has been attached a card or slip, and requested to fill out the necessary information. 10. Many doctors feel that a questionnaire should be presented to the patient only after the initial history has been obtained and a positive rapport has been established between doctor and patient. 11. The doctor's actual examination has begun with a review of the initial data. 12. If the complaint is chronic in nature, the doctor will reflect on what he has learned of the natural progression of such a syndrome in a similar situation. 13. Deep probing into the patient's chief complaint will frequently uncover diseases and disorders that were predestined in years past and could have been avoided or minimized if an efficient case history had been obtained at that time. 14. Once the chief problem has been defined, the patient should be encouraged to offer more details of the situation. 15. If the patient has been involved in trauma, shock, or a crisis, it is not unusual for a degree of amnesia or faulty recall to be present. 16. If you ask most lay people, "Have you ever had jaundice?", most will respond, "No". 17. Studies have shown that a physician's interest, acceptance, recognition, and empathy are more important to the patient in selecting a doctor than the physician's technical and scientific ability. 18. When information about the patient has been tabulated, it must be reviewed in light of the doctor's basic science knowledge and clinical experience. 19. Ask the patient to describe the symptom or problem that brought them to hospital by using an open ended question: “What has happened to bring you to hospital?” or “What seems to be the problem?” 20. Once you have determined what the presenting complaint is, it must be evaluated in detail. 21. Sometimes the patient will tell you the diagnosis: “The doctor said that I've got pneumonia.”
|
|
|

Review your progress
Test for self-control
Grammar
|
|
|


